Knowing the foods that cause your child’s food allergy reactions can help you best manage their allergy, reduce stress, and avoid restricting their diet unnecessarily. To help diagnose a food allergy, an allergist may recommend allergy tests.
But allergy tests only tell part of the story. Instead, food allergy tests work with your child’s personal, medical, and symptom history to help your child’s doctor confirm their allergens.
What Do Food Allergy Tests Look For?
There are two categories of food allergies:
- Immunoglobulin E (IgE) mediated – a type of allergy that has the potential to cause a severe allergic reaction called anaphylaxis
- Non-IgE-mediated – a type of allergy that usually affects the digestive tract (gut), such as eosinophilic esophagitis (EoE) and food protein-induced enterocolitis syndrome (FPIES)
Food allergy tests are best for IgE-mediated food allergies. They are rarely recommended for non-IgE-mediated food allergies.
What Are the Most Commonly Used Food Allergy Tests?
There are four types of food allergy tests that are most often used by allergists:
- Skin prick test
- Specific IgE (sIgE) blood test
- Component test
- Oral food challenge
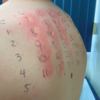
Skin Prick Test
Skin prick testing (SPT) is one of the most commonly used allergy tests. You may have heard it called a “scratch test.” With SPT, the allergist places a drop of an allergen on your child’s skin and the lightly pricks it. This causes the allergen to go into the top layer of the skin.

If your child has IgE antibodies – immune cells that react with an allergen and cause an allergic reaction – to the food, they will develop a red, itchy bump. This bump is called a wheal or a flare.
Just because your child reacts to the allergen doesn’t mean they are allergic to the allergen. But if your child has had symptoms in the past when eating the allergen, SPT can help confirm the allergy.
Specific IgE Blood Test
The specific IgE (sIgE) blood test measures levels of specific IgE in the blood for certain foods. This test was previously known as RAST or ImmunoCAP testing. The allergen will be introduced into a sample of your child’s blood to see if IgE antibodies are found.
Like SPT, a positive result doesn’t mean your child is allergic. It can be used to confirm a diagnosis if other factors suggest an allergy. Also, the results – or “class levels” – don’t relate to whether or not your child is more likely to have anaphylaxis. Your child can have a low class level and still have a severe allergic reaction.
Component Test
A component test is another type of blood test. It’s different from other tests because it looks at IgE levels in the blood to different proteins in a food instead of the whole food. These tests are designed to try and determine if your child’s IgE tests are elevated due to true food allergy or are false positives from cross-reactivity with inhalant allergens.
Oral Food Challenge (OFC)
The best way to know if your child is actually allergic to a food is to have them eat it during an oral food challenge (OFC) in an allergist’s office. It’s the gold standard for confirming whether or not your child has a food allergy.

In an OFC, your child eats small, increasing amounts of their suspected food allergen. The allergist and their staff watch your child for a reaction and are prepared to treat any symptoms, if they arise. It’s the most reliable allergy test for food allergies.
What Should I Do If I Think My Child Has a Food Allergy?
If you think your child has a food allergy, see a board-certified allergist, if possible. They know how to look at your child’s full history along with allergy tests to confirm or rule out a food allergy. Avoiding foods without a proper diagnosis can lead to issues like food anxiety, poor quality of life, and poor nutrition – factors that can have a major impact on your child’s well-being, health, and development.
Medical review: June 2023 by David Stukus, MD
It is important to stay up to date on news about food allergies. By joining our community and following our blog, you will receive news about research and treatments. Our community also provides an opportunity to connect with other people who manage food allergies for support.



Comments (46)