Update – Aug. 21, 2020
Sixteen leading food allergy experts, including some of our medical advisors, released school guidelines addressing food allergies in light of COVID-19. We have added those recommendations to this blog post.
Schools face major challenges as they try to reduce the spread of the coronavirus that causes COVID-19 among staff and students. Schools will follow certain policies and practices to help reduce the spread. This causes many parents to wonder how this will affect their child with food allergies or asthma.
Most school districts have policies about face masks, physical distancing, and cleaning. These policies may affect how schools handle food allergies. But in most cases, the impact on kids with food allergies should be minor. In fact, some policies may enhance prevention of food allergic reactions. Here are how some COVID-19 policies may impact food allergy management:
- Face masks – Overall, wearing a face mask should not have much impact on food allergy management. Parents and teachers should remind kids to not share masks to prevent both COVID-19 and food cross-contact. If you supply masks for your child, write their name on the inside with a laundry marker to make sure they can always identify their mask.
- Physical distancing – Keeping kids apart should reduce the chances for food sharing and accidental food cross-contact at mealtimes.
- Classroom meals – Some schools may serve meals in the classrooms. Kids may be separated due to physical distancing. This can reduce food sharing and cross-contact. Schools should empower teachers to read labels to identify food allergens. Kids With Food Allergies (KFA) has guides on how to read food labels. Teachers should also discourage food sharing to prevent both food allergy reactions and COVID-19.
- Handwashing – Frequent handwashing, especially before and after eating or touching food, has always been encouraged to prevent food allergy reactions. Many schools are requiring more frequent handwashing to reduce the spread of the coronavirus. This can also lower the chance of food cross-contact on shared surfaces.
- Increased cleaning – Schools have increased cleaning to reduce the spread of the coronavirus. Cleaning more often can also reduce the spread of food particles. To also reduce the chance of food allergy reactions, schools should clean desks before and after meals and snacks.
What Parents Can Do to Prepare for the New School Year
Start the process now to get your child’s school health forms signed. Contact your school to get the current copies of their forms. And then call your child’s doctor to get them signed. Make plans now so you can submit the signed forms to the school as soon as possible.
If your child has a school care plan such as a 504 plan, contact the school to find out if policy changes will affect the plan.
Help your child prepare for the new school year now:
- Have them practice wearing a mask so they can become comfortable with one.
- Teach them how to wash their hands properly.
- Encourage them to tell an adult if they have any symptoms (such as their mouth feels funny, they are itchy, their throat hurts, etc.). Try some role-playing to help your child practice.
Guidance for Schools on Food Allergies, Asthma, and COVID-19
There are several resources schools can use to protect students and staff with food allergies and asthma during the COVID-19 pandemic.
The Centers for Disease Control and Prevention (CDC) has guidance for schools during the COVID-19 pandemic. They encourage schools to keep food allergies in mind when creating policies. The CDC also offers general guidance schools can follow to manage food allergies, called “Voluntary Guidelines for Managing Food Allergies In Schools and Early Care and Education Programs.”
Sixteen food allergy experts released recommendations for how schools can handle food allergies in light of COVID-19 policies.
They created eight recommendations for schools:
- Before and after meals, wash hands with soap and water and clean surfaces. Don’t allow food sharing.
- Remember that food allergen bans are not medically necessary and should not be included in 504 plans. They do not decrease the risk of anaphylaxis, a severe allergic reaction.
- Make reasonable changes to 504 plans to work with school recommendations.
- Stock epinephrine in all schools. Consider plans to keep student epinephrine in their classrooms when possible.
- Train all school staff to recognize and treat food-allergic reactions, including anaphylaxis.
- Create a zero-tolerance policy for food allergy bullying.
- Consider modified approaches in individual schools and classrooms based on special situations.
- Communicate clearly with food allergy parents and encourage open discussion.
The recommendations also outline everyone’s role in managing food allergies in schools during the COVID-19 pandemic.
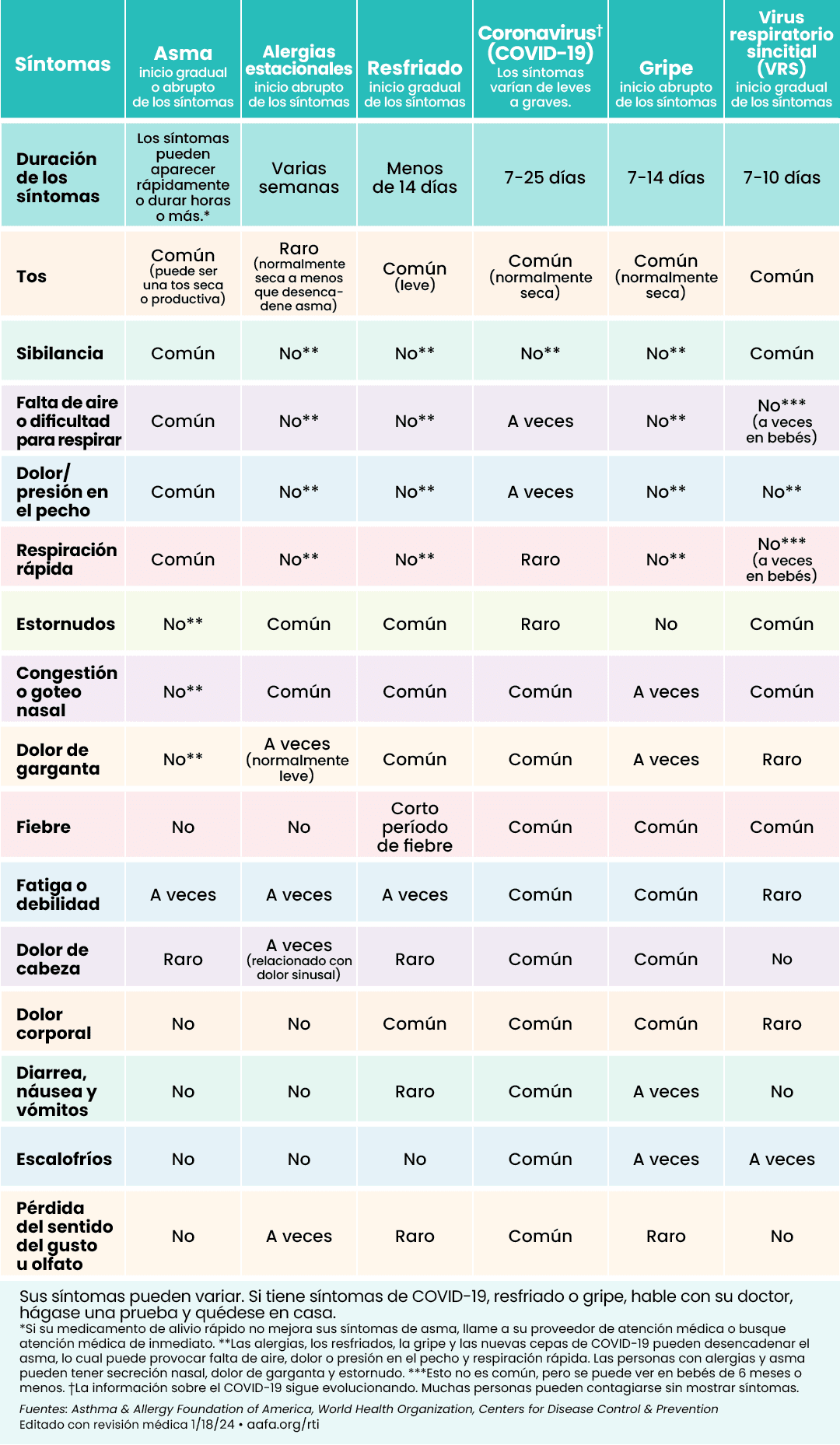
The Asthma and Allergy Foundation of America (AAFA) also created a COVID-19 and Asthma Toolkit for Schools. This resource supplements current district, state, and federal guidelines. It has resources to help schools better manage asthma and while addressing the COVID-19. It also has AAFA’s “Is it COVID-19, the Flu, a Cold, Allergies, or Asthma?” symptoms chart for quick reference (in English and Spanish) and a list of resources.
The toolkit includes easy-to-use checklists schools can use daily to manage asthma and minimize the spread of the coronavirus.
While increased cleaning can help reduce the spread of the coronavirus, it can be an asthma trigger. Asthma is a leading chronic disease in children. There is a good chance nearly every U.S. classroom has a student with asthma. Many staff members have asthma too.
Schools should take special care to clean in a way that reduces the spread of the coronavirus but doesn’t increase asthma symptoms in staff and students. Teachers and staff should not bring in cleaning or disinfecting products from home to avoid the risk of mixing chemicals. Only use district-approved and provided products. Children should not be allowed to clean any hard surfaces in the classroom.
School staff should also remember cleaning and disinfecting are not the same. Some cleaners clean and some disinfect. Clean first to remove particles and residue (including food) from surfaces. Then disinfect to remove possible virus particles.
 You can access AAFA’s free COVID-19 and Asthma Toolkit for Schools two ways:
You can access AAFA’s free COVID-19 and Asthma Toolkit for Schools two ways: Sign up to receive your copy. You will be alerted if any changes are applied to the toolkit or future editions are released.
Kids With Food Allergies is a division of AAFA.


Comments (5)