PRESS RELEASE
Study Finds Cause of Mysterious Food Allergy, Suggests New Treatment Strategy
CINCINNATI, July 13, 2014 /PRNewswire-USNewswire/ -- New research in Nature Genetics identifies a novel genetic and molecular pathway in the esophagus that causes eosinophilic esophagitis (EoE), opening up potential new therapeutic strategies for an enigmatic and hard-to-treat food allergy.
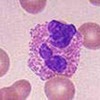
EoE is a chronic inflammatory disorder of the esophagus. The condition is triggered by allergic hypersensitivity to certain foods and an over-accumulation in the esophagus of white blood cells called eosinophils (part of the body's immune system). EoE can cause a variety of gastrointestinal complaints including reflux-like symptoms, vomiting, difficulty swallowing, tissue scarring, fibrosis, the formation of strictures and other medical complications.
Reporting their results online, the multi-institutional team of researchers was led by scientists at Cincinnati Children's Hospital Medical Center. The authors identified a molecular pathway specific to epithelial tissue in the esophagus involving a gene called CAPN14, which they found becomes dramatically up-regulated in the disease process.
Epithelial cells help form the membrane of the esophagus. The scientists report that when these cells were exposed to a well-known molecular activator of EoE – an immune hormone called Interleukin 13 (IL-13) – it caused dramatic up-regulation of CAPN14. The researchers said this happened in what they described as an epigenetic hotspot for EoE on the cells' chromosomes.
CAPN14 encodes an enzyme in the esophagus that is part of the disease process called calpain14, according to Marc E. Rothenberg, MD, senior investigator on the study and director of the Center for Eosinophilic Disorders at Cincinnati Children's. Because caplain14 can be targeted and inhibited by drugs, the study opens up new therapeutic strategies for researchers.
"In a nutshell, we have used cutting edge genomic analysis of patient DNA as well as gene and protein analysis to explain why people develop EoE," Rothenberg explained. "This is a major breakthrough for this condition and gives us a new way to develop therapeutic strategies by modifying the expression of caplain14 and its activity. Our results are immediately applicable to EoE and have broad implications for understanding eosinophilic disorders as well as allergies in general."
The study follows years of research into EoE by Rothenberg's laboratory, including the development of novel modeling systems for the disease, and extensive multi-institutional collaboration through the National Institutes of Health's Consortium of Food Allergy Researchers. Other key collaborators on the current study include first author, Leah Kottyan, PhD, a researcher at the Center for Autoimmune Genomic Etiology at Cincinnati Children's, and co-senior investigator John Harley, MD, PhD, director of the Center of Autoimmune Genomic Etiology .
Rothenberg's lab years ago identified IL-13 as a key molecular contributor to the allergic reaction process in EoE. His team has since identified a number of related genes and molecular pathways linked to the disease, and they have tested drugs that inhibit IL-13 in an attempt to manage EoE severity.
"The current study links allergic responses mediated through IL-13 with an esophageal specific pathway, and answers a long-standing question in the allergy field of why people develop tissue specific disease manifestations," Rothenberg explained. "We have uncovered that this can be explained by the interplay of genetic susceptibility elements in allergic sensitization pathways with the newly discovered esophageal specific pathway. Thus, two steps are necessary, one dictated by allergy and one dictated by calpain14 in the esophagus."
The researchers used computer bioinformatics to conduct a genome-wide association study that analyzed 2.5 million genetic variants in thousands of individuals with and without EoE. This allowed the authors to identify the genetic susceptibility within the CAPN14 gene. The investigators were surprised to learn that CAPN14 was specifically expressed in the esophagus, compared with 130 other tissues in the body they analyzed.
Rothenberg said the findings open a new way to consider therapeutic options because calpain14 is an enzyme that can be inhibited by drugs, which means it may be possible to modify the expression and activity of calpain14. Some chemical compounds already exist that block the activity of calpains, although the researchers do not yet know the exact function of calpain14, as very little has been published about it.
Funding support for the study came in part from the National Institute of Allergy and Infectious Disease, the National Institute of Diabetes and Digestive and Kidney Diseases, the National Heart, Lung and Blood Institute, the National Human Genome Research Institute, the National Center for Research Resources (grant numbers U19 AI066738, U01 HG006828, U01 HG006828-S1, U01 HG006828-S2, U01 AI066560, R37 AI024717, P01AI083194, T32 HL7752-19, K23 AI099083, P01 AR049084, TR001082, UL1 TR-000067, UL1 TR-000039, UL1 TR-00083, UL1 TR-000424), the Department of Veterans Affairs (IMMA 9) and the Department of Defense (PR094002).
Additional support came from the Campaign Urging Research for Eosinophilic Diseases (CURED), the Buckeye Foundation, the Food Allergy Research Education (FARE) foundation and the Foundation of the American College of Allergy, Asthma, and Immunology.
Other NIH Consortium of Food Allergy Researchers institution collaborating on the study included: the Icahn School of Medicine at Mount Sinai, New York; Johns Hopkins University School of Medicine, Baltimore; University of Arkansas for Medical Sciences and Arkansas Children's Hospital, Little Rock, Ark.; the University of North Carolina, Chapel Hill, N.C. and National Jewish Health in Denver, Col.
About Cincinnati Children's: Cincinnati Children's Hospital Medical Center ranks third in the nation among all Honor Roll hospitals in U.S.News and World Report's 2014 Best Children's Hospitals. It is also ranked in the top 10 for all 10 pediatric specialties. Cincinnati Children's, a non-profit organization, is one of the top three recipients of pediatric research grants from the National Institutes of Health, and a research and teaching affiliate of the University of Cincinnati College of Medicine. The medical center is internationally recognized for improving child health and transforming delivery of care through fully integrated, globally recognized research, education and innovation. Additional information can be found at www.cincinnatichildrens.org . Connect on the Cincinnati Children's blog, via Facebook and on Twitter

Comments (0)