In August 2019, the Asthma and Allergy Foundation of America (AAFA) released their My Life With Food Allergy Parent Survey Report. (Kids With Food Allergies is a division of AAFA.) The report highlights the significant social, emotional and financial impact food allergies can have on parents.
Our findings also revealed that many children did not receive epinephrine when they were having a severe allergic reaction for many reasons. We asked Dr. Michael Pistiner, pediatric allergist at MassGeneral Hospital for Children in Boston, Massachusetts, to talk about these findings and using epinephrine. He also offered thoughts on how parents can reduce fear and worry and teaching children self-management.
AAFA: AAFA’s My Life With Food Allergy Parent Survey found that many parents feel fearful or worried for their child’s safety because of their food allergy. What can help parents feel more confident and lessen their concerns?
Dr. Pistiner: The first thing parents can do is get comfortable with basic food allergy management. The pillars of food allergy management are prevention and emergency preparedness. These pillars should be maintained at all times and in all circumstances.
To prevent allergic reactions, whoever is preparing and serving food must understand how to read labels, how to prevent cross-contact and how to clearly communicate about the child’s allergy. Anyone caring for a child with a food allergy will need to know how to recognize anaphylaxis, a severe allergic reaction. They will need to have epinephrine available. And they need to be able to effectively give the child epinephrine and contact emergency services.
Once families get comfortable with basic food allergy management strategies, then these can be applied to all settings, including travel, drop-off playdates, etc. Effective food allergy management can be done while, at the same time, maintaining excellent quality of life and not compromising a child’s ability to have fun and learn.
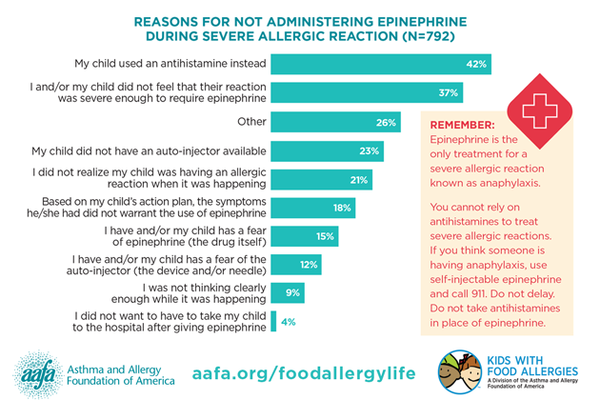
AAFA: In AAFA’s survey, when asked if their child has ever experienced an allergic reaction that the parent would consider severe, 1,095 respondents (90%) reported that it happened at least once. Of those 1,095 parents whose child had experienced at least one severe allergic reaction, nearly three out of four (72%) said their child has experienced a severe allergic reaction and epinephrine was NOT administered. What are the guidelines for identifying and treating anaphylaxis? Is it concerning that 72% of parents report their child did not receive epinephrine when the parent thought they were having a severe allergic reaction?
Dr. Pistiner: Epinephrine is a safe medicine, and it is the first line and only main treatment for anaphylaxis. It works fast, it works on all of the symptoms caused by anaphylaxis and it is safe.
We ask that people call an ambulance after its use because we don’t want to slow down giving the epinephrine. It’s not that epinephrine makes it so we have to call an ambulance. We call an ambulance because of the reaction itself. Also, the ambulance is bringing things that make epinephrine work better, like oxygen and IV fluid, in addition to more epinephrine and more people.
One really important and helpful tool is the anaphylaxis emergency care plan, sometimes also known as an anaphylaxis action plan, food allergy action plan or food allergy emergency care plan. This is a document that is signed by the child’s health care provider and parents. It is an incredibly helpful tool to have available with the child in addition to their epinephrine auto-injectors at all times and in all circumstances. Essentially, this is a cheat sheet for when to use epinephrine. It lays out the different signs and symptoms the child may experience. And if these are present, then the plan tells you what to do.
Current plans will recommend the use of epinephrine for certain severe symptoms and/or combination of mild symptoms.
There is an action plan from the American Academy of Pediatrics (AAP) that has also been approved by National Association of School Nurses (NASN). Following such plans can help ensure that if someone were experiencing symptoms that could be part of a severe allergic reaction, then the child would receive epinephrine.
This My Life With Food Allergy Parent Survey Report did a great job starting the conversation about why people may not give epinephrine. If it’s the first time a person had an allergic reaction, then clearly they wouldn’t have it and it wouldn’t have been available.
Another thing that came up in this survey is that if you took 100 parents and ask them what was severe, you might get many different answers. Again, this is where these action plans can be really helpful. They put us on the same page. The bottom line in the goal of these action plans is that when there are signs and symptoms that can suggest anaphylaxis, then the next step is to give epinephrine. Please see HealthyChildren.org on anaphylaxis action plans.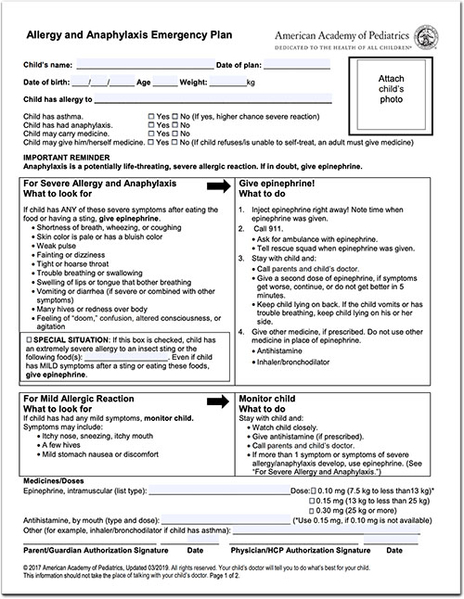
AAFA: Of the 792 people who reported their child did not use epinephrine for treatment of a suspected severe allergic reaction, 42% said their child used an antihistamine (such as Benadryl) instead. What is the role of antihistamines in treating allergic reactions from food? What do parents, school staff and first responders need to know about antihistamines and anaphylaxis?
Dr. Pistiner: I like to consider antihistamine comfort medicine. It is appropriate to use an antihistamine for a mild reaction. It’s important to know that antihistamines don’t decrease the chance that a reaction will turn into anaphylaxis. And it won’t make an anaphylactic reaction any less severe. It’s helpful to think of epinephrine as the emergency medicine and antihistamine as comfort medicine. Antihistamine is not emergency medicine and would never be used in a way that could possibly delay the use of epinephrine. Epinephrine works quickly and everywhere we want it to.
Past studies have shown you can get peak levels of epinephrine in eight minutes, and it can start working even faster than that.
Antihistamines take 30 to 60 minutes to start working.
Epinephrine works on the heart, lungs, blood vessels, gut – really everywhere we need it to when we’re having an allergic reaction. Antihistamine works well on skin and mucosal surfaces.
AAFA: According to AAFA’s survey, only half of parents report they feel very confident in knowing which emergency medicines to administer and when for food allergic reactions (page 15). Less than one-fourth of adult patients report feeling very confident about the same. Only 42% of parents and 19% of adult patients feel very confident in administering an epinephrine auto-injector. How can we improve confidence levels for parents and patients?
Dr. Pistiner: We just covered when epinephrine should be used, but the next issue is going to be how to give it. Not only will a caregiver of a child with a food allergy need to feel confident knowing when to give epinephrine, but they’ll need to feel confident knowing how to give epinephrine. And epinephrine needs to be available in the form they were trained to give.
The key is going to be practice and training. It’s really helpful to use a training device which is a fake auto-injector that someone can practice on. Each of the auto-injector companies makes trainers. It would be really great if whenever someone was prescribed an auto-injector they were trained on the auto-injector they were given by their pharmacy.
Currently, there are five different models of auto-injectors available, in addition to a prefilled needle and syringe. This can add to the confusion. Sometimes a health care provider might prescribe one type and the pharmacy only has another type of available. Ultimately, the family needs to be trained on the device they wind up having available for their child. Also, they will need to be able to train any other caregiver of that child they’re passing off responsibility too. Therefore, it’s going to be essential for the parents to have training devices available to train secondary caregivers like babysitters, relatives and others.

AAFA: At what age should parents and caregivers start teaching children with food allergies to understand when and how to use their emergency medicines so they have confidence when they are independent adults caring for themselves?
Dr. Pistiner: A way to start thinking about this is that we need kids to be able to self-manage when they are going to be alone. Each individual child is going to be a bit different. Some might be at an earlier age and some at a later age, depending on their own confidence and their own developmental capabilities. Something to keep in mind is that we want a gradual increase in responsibilities and enough time for practice so the child can get comfortable before it really matters.
For the younger children, it may be just understanding what a grownup might be thinking when it comes to their emergency medicine. They simply need to know emergency medicine goes with them wherever they are, whoever they’re with. Their emergency medicine will make them feel better quickly if they had an allergic reaction and they needed it. For some kids, medical play can be really helpful to get them comfortable and understanding.
Answering their questions honestly also goes a long way in adding to comfort. Also, taking care of misinformation and assumptions that might create fear will be really helpful. When some younger children look at auto-injectors, they may just assume the needle length is the length of the device. It is often very reassuring to correct them and let them know the actual needle is in fact very short and very skinny.
In order to be able to self-administer, a child would need to know what signs and symptoms to look for. Also, they would need to be able to follow all the necessary steps to administer the device. When I talk to families or think about it in the context of my own child, self-administration becomes something I train for when the child is developmentally at the stage where they’re not going to be under the supervision of a trained grownup. For example, hanging out with friends, staying in the house by themselves, going to someone else’s house where only children are present, etc. In these circumstances, if a child is not developmentally ready or able to be trained, then they shouldn’t be without a grownup who would be able to recognize anaphylaxis and administer epinephrine. For some, this may be age 12 or 13. For some kids, depending on the circumstances, it could be sooner or later. We never want to force a child to feel responsible or be responsible before they’re emotionally or physically ready for a task like this that can cause anxiousness and concern.
AAFA: Any other thoughts about AAFA’s My Life With Food Allergy Parent Survey Report that you’d like to share?
Dr. Pistiner: This survey does a really good job in starting excellent conversations with the health care team and with experts like AAFA. For health care providers, it helps us know what some of the important talking points should be when educating and supporting the families we care for.
It also does a good job starting important conversations and helping health care providers educate and empower in an effective way that is then specific to that family and child.



Comments (0)